Strictly speaking, self-injury is not a symptom of autism. However, certain symptoms, situations, and comorbidities related to ASD can lead some people with autism to engage in self-injurious behavior. Treating underlying disorders and helping the individual to learn additional communication and coping skills can enable them to avoid self-injury and minimize the long-term effects of this behavior.
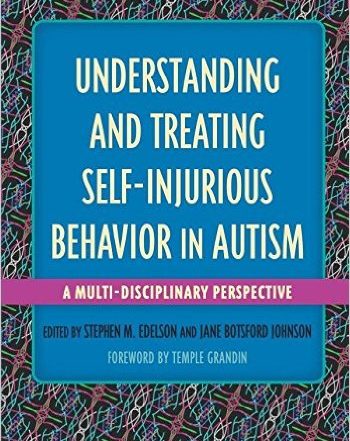
With contributions from the leading experts in research and treatment, Understanding and Treating Self-Injurious Behavior (2016) provides a comprehensive analysis of this poorly understood behavior in people with Autism Spectrum Disorder (ASD) or related developmental disabilities, and the different methods available to treat them. The book is edited by ARI’s executive director, Stephen M. Edelson, and past ARI Board member, Jane B. Johnson, and consists of chapters written by leading experts in the autism field. Learn More
What is self-injurious behavior
It is important to remember that individuals may engage in self-injury for many reasons. This article deals specifically with self-injury co-occurring with autism. However, people with other conditions may also engage in self-injury.
Any behavior that causes physical harm to the individual is classified as self-injurious. This could include:
- Slapping
- Scratching
- Headbanging
- Biting
- Pinching
To address these behaviors, caregivers must first understand the underlying issues that may be causing them.
Why do some people with autism engage in self-injury?
People often view self-injury in terms of its effects. A child may suffer a lasting injury, and a parent may feel demoralized or overwhelmed, and strangers may not understand. While these effects can grab attention, focusing on them is unlikely to address the underlying issue. Parents and clinicians aiming to help a person diagnosed with autism who is engaged in self-injury should start by investigating triggers that lead to the behavior. Often self-injury can begin accidentally and, when it’s inadvertently reinforced, it can become a learned behavior.
In many cases, self-injury serves as a means of communication. Often a child is trying to convey a feeling or idea they may not be able to express in words. Biting, headbanging or other self-injurious behaviors are a means of getting their needs met and may be their urgent need to express pain, fear, displeasure, or anxiety. They may be trying to say, for example, “I’m scared, I want to get out of here” or “this is too hard, I don’t want to do this” or “Play with me!” or “Look at me!” or “My head hurts, it feels better when I bang it,” etc.
Self-injury can also be a form of sensory stimulation. An individual with autism may self-injure as a way to increase or decrease their level of arousal.
Often, self-injury is a learned behavior. Parents certainly don’t intend to teach children to engage in self-injury, but they may unintentionally reinforce the behaviors. If the child engages in self-injury and the parent or teacher hands them a preferred toy, the child quickly learns that self-injury leads to their favorite toy. On the other hand, if the child engages in self-injury, and the parent immediately removes them from an overstimulating environment, they learn that self-injury can help them avoid uncomfortable situations.
Lauren Moskowitz, Ph.D., explores the motivations and reasons for such behaviors in her webinar Assessing and Treating Challenging Behavior in Individuals with ASD.
It is important to remember that the child is not acting with malice, and neither is the parent or caregiver. In both cases, the child is attempting to communicate very real wants and needs. When the behavior achieves the result they wanted, they learn to associate self-injury with a positive result. Their goal is not to anger or manipulate. Instead, they are attempting to communicate. If self-injury achieves their goals, they are likely to continue the behavior.
Other factors that may be associated with self-injury include biochemistry in the brain, seizure activity, genetic factors, a pain response, or frustration. Dr. Stephen M. Edelson explores the research behind these factors in his article on Understanding and Treating Self-Injurious Behavior.
Identifying the causes of self-injury
Before you and your care team can identify interventions that are likely to address self-injury, you will need to understand the reasons and motivations for the behavior. What does the child need or want? What communication barriers do they face that led them to initiate the behavior? When you identify situations or stimuli that are likely to trigger episodes of self-injury, you can begin to understand what the individual is attempting to communicate.
Parents and caregivers can keep a journal to track instances of self-injury, including where it occurred, what was happening, who was present, what occurred immediately before, what occurred immediately after – e.g., how did other people react/respond, did the child get to avoid or escape or leave or delay a difficult situation – etc. Written records are more reliable than emotionally charged recollections, and can help you notice details you might otherwise have passed over.
Your clinician may use a functional behavioral assessment (FBA) to help identify the function of self-injurious behavior for the individual. This process includes:
- Defining the behavior: using specific, observable language to describe what the self-injury looks like
- Gathering and analyzing information: exploring when, where, and how the behavior is occurring, the consequences of the behavior, and the people and situations that seem to be related.
- Identifying reasons or causes: making an informed hypothesis about what might be causing the behavior or what the child is trying to communicate.
- Making a plan to address the situation: specifying actions and interventions to help improve communication or reduce trigger events.
Teachers and school officials also use this method to identify ways to better support students. The result is a behavior intervention plan (BIP) that guides them to teach and reward positive behaviors.
Interventions to address self-injury
The most important thing you can do is teach the child to communicate
Once you understand what is causing the behavior, you can work with your clinician and make a plan to address it.
If the self-injury is related to anxiety or discomfort in certain situations, social stories and priming may help ease transitions. Social stories help children practice before a situation occurs in real life, and priming provides the child with information about what will happen next to reduce their anxiety. Providing choices can also give the child a venue to communicate needs and preferences. Anything that makes situations more predictable, such as priming and social stories, can be helpful in reducing self-injury for those people with ASD for whom unpredictability serves as a trigger for the self-injury.
Teaching an alternative behavior to replace the self-injury to help the child get their wants and needs met in another way is crucial. For example: if a child bites his hand and, subsequently, his parents leave him alone whenever he bites his hand (i.e., the self-injury serves an escape function), then the most important intervention is to teach the child the words to use instead. Teaching him to say “leave me alone,” or something equivalent to that – either verbally or through sign language or with PECS or an ACC device, etc. – empowers him to have his needs met in a safer way.
The second most important thing is to remove or alter the triggers. Social stories and priming can help make things more predictable if the trigger is unpredictability, but if the trigger is – for example – a math assignment that is too hard for the child, then you need to make the math assignment easier or provide more help.
The third most important thing you can do is reinforce the child for displaying communication instead of self-injury… and/or reinforce the child for periods of time in which he/she displays reduced occurrences and, eventually, no self-injury.
Treating physical ailments
In some cases, children will engage in self-injury to communicate that they are feeling physical pain or discomfort. For example, you might assume that a person may bang their head because they have a headache. However, sometimes the action and the pain are not so closely related. Headbanging can be a sign of gastrointestinal issues or other discomforts as well. A careful medical examination with a physician who is knowledgeable about autism and its co-occurring conditions is crucial to identifying physical ailments that may be an underlying cause of the behavior.
Exploring psychological causes
Anxiety and depression are both common comorbidities of autism. Look for other signs like changes in sleep, mood, or energy that may indicate a psychological comorbidity. Treating these disorders may help to minimize or prevent self-injury.
Behavior therapy
If the self-injury has become a habit, then behavioral therapy may help children replace old self-injurious patterns with new skills and strategies. By rewarding positive behaviors and teaching new communication and coping skills, behavior therapy may help some children cease self-injurious behavior.
For a deeper look at self-injurious behavior, its causes, and its interventions, explore this article from Stephen M. Edelson, Ph. D.
ARI thanks Lauren Moskowitz, PhD, for her contributions to this article.
Introducing: ARI’s Understanding and Treating Self-Injurious Behavior Tool
This free resource provides deeper insight into understanding and treating self-injurious behavior in autism. It is designed to assist professionals and parents in identifying treatments that may reduce or eliminate self-injurious behaviors (SIB) in clients or children. Filling out the questionnaire may provide insight into one or more possible reasons why an individual engages in SIB. Links to published studies on causes as well as appropriate interventions, are also provided.
Wellbeing Wins: Integrating Positive Psychology into the Autism Community
Free webinar at 1 p.m. Eastern time (US), Wednesday, September 25, 2024 About the speaker: Patricia Wright, PhD, MPH, is Executive Director of Proof Positive: Autism Wellbeing Alliance.
Sexual Victimization in Autism
In this article: Chronic maltreatment and sexual victimization Trauma and quality of life Risk Factors What can we do? A safer future Resources Despite evidence to the contrary, misperceptions of autistic
Autism and Pica
Dean Alexander, Ph.D., discusses pica, the ingestion of non-food substances, which has received insufficient attention as a common, sometimes lethal, form of self-injurious behavior. He discusses the prevalence of pica in autistic
Early exposure to pollutants may alter brain’s development
A new study suggests that exposure to air pollutants before birth and during childhood may lead to alterations in white matter microstructure in the brain. Abnormal white matter microstructure has been
Understanding and Treating Autism: Book Series
A new book, titled Understanding and Treating Sleep Disturbances in Autism, is now available from Jessica Kingsley Publishers. The book is edited by ARI's executive director, Stephen M. Edelson, and past ARI
Understanding and Treating Self-Injurious Behavior in Autism
Pictured: Editors Stephen M. Edelson and Jane Botsford Johnson A comprehensive, authoritative resource on understanding and resolving self-injurious behavior (SIB) in people with autism and related conditions with contributions by top