Dr. Calliope Holingue, MPH, Ph.D., provides an overview of the intersection between the gut, autism, and well-being. She outlines recent studies on the GI needs and experiences of autistic individuals and discusses the complex pathways of connection between the gut and autism. The presenter summarizes GI-autism research to date, highlighting the need for screening tools specific to autistic GI experiences. Diet change and Fecal Matter Transplant are outlined as microbial interventions in autism. Holingue provides tips for recognizing GI distress and discusses future directions for research and interventions before the Q&A.
In this webinar:
1:00 – Outline
1:50 – Autism and gastrointestinal issues
4:15 – Common GI symptoms
6:20 – Study: Qualitative study of families with autistic children with GI issues
12:00 – Study: GI experiences and needs of autistic adults
16:20 – Linking GI symptoms and autism
21:04 – Intersection of autism and GI research
25:55 – Microbiome interventions in autism
32:10 – Fecal matter transplant (FMT)
34:00 – Study: Autism and microbiota transfer therapy
39:55 – Recognizing GI distress in autism
43:05 – Quotes from parents
44:24 – Gastrointestinal and related behaviors inventory (GIRBI)
45:50 – Future directions
47:45 – Q&A
Autism and gastrointestinal issues
Holingue outlines common clinical characteristics of autism and explains how co-occurring medical conditions affect autism heterogeneity (1:50). People with autism often have complex healthcare needs but consistently experience a lower quality of care and assistance across their lifetime (3:05). The speaker explains that gastrointestinal (GI) issues like constipation, diarrhea, and abdominal pain are incredibly common in autism, occurring in 47% of autistic participants in a recent meta-analysis (4:15). She notes that GI distress has been linked to co-occurring conditions like seizures, sleep disorders, and functional behavior difficulties (5:30).
Study: Qualitative assessment of GI issues in autistic children and their families
The speaker outlines her 2022 publication in Autism, assessing the experiences of autistic children with GI issues and their families. Researchers derived four main themes from 12 parent interviews (6:20). First, autistic children often have difficulty verbally communicating the presence of GI symptoms, and second, GI issues impact a child’s overall well-being and ability to fully engage in activities like school or social gatherings (7:40).
The third theme to emerge was how GI issues impact the family’s well-being due to parental frustrations, financial stressors, and limitations on family activities (9:00). Finally, theme four highlights the challenges parents experience with finding accessible quality care for their children. Many noted lengthy, complicated processes, medical offices not conducive to autism, and a lack of education and experience in healthcare providers (10:12).
Study: GI experiences and needs for adults with autism
Holingue outlines a study exploring the GI experiences of autistic adults (in preparation for publication). The study aims to investigate the needs and priorities of autistic adults and develop recommendations for research and support (12:00). Similar to the first study, participants said that GI symptoms profoundly impact their ability to create relationships, work, and live comfortably (overall well-being). They also described common triggers for GI issues, including stress, sensory overwhelm, and changes in routine, and highlighted frustrating and unhelpful experiences with the healthcare systems (13:15). To improve GI health in autistic adults, the researchers recommend more training around interoception, anxiety, and advocacy for adults with autism. Similarly, they assert the need for increased healthcare provider training on assessing and treating complex health issues and autism accommodations (15:15).
The intersection of autism and GI issues
Pathways of connection
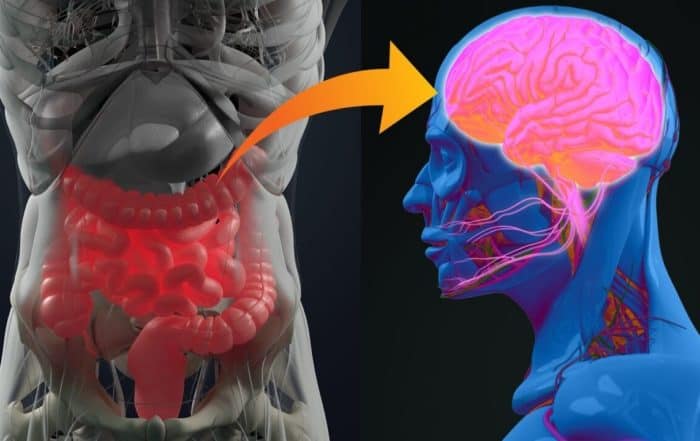
Holingue claims that pathways linking autism and GI issues are complex. For example, common co-occurring conditions, like anxiety, sleep problems, and restrictive diets, drastically alter the gut microbiome (16:20). Similarly, GI symptoms can exacerbate irritability, anxiety, and other behaviors related to pain or discomfort (19:00). The presenter touches on biological pathways that interact with GI health including the microbiome, vagus nerve, immune system modulation, gut permeability, and serotonin production (20:14). She explains that maternal microbiomes interact with fetal immune systems and how early life exposures shape the development of the microbiome (i.e., delivery mode, diet/breastfeeding) (29:00).
History of GI-autism research
The speaker outlines autism-GI research starting from the early 2000s. She briefly summarizes initial observations (21:04), the discovery of the gut-brain axis (22:15), how microbiome diversity can inform behavior and treatment (22:40), and the beginning of intervention studies (23:35). Contemporary research, Holingue continues, focuses on understanding the mechanisms by which the gut microbiome influences the brain and how the environment influences the composition of the gut microbiome (24:30).
Microbiome interventions in autism
Microbial interventions hold promise in autism because they are modifiable for individuals across heterogeneities. The speaker notes that most studies to date are strictly pediatric (25:55). Findings across the field are divergent and inconclusive due to small cohorts, different comparison groups, and autism heterogeneity (26:30). The presenter asserts that failure to control for potential confounders, or other things that could impact the microbiome (i.e., diet, antibiotics, medications, etc.) is a major limiting factor across studies.
Diet change is a common intervention that affects gut microbial composition (30:50). Holingue describes fecal matter transplant (FMT), where a healthy donor provides feces (after extensive screening and safety measures), which contains microbiota needed by someone with a specific health condition. The cleaned microbiota is delivered to the recipient via pill, drink, or endoscopy (32:10). She discusses the difference between intestinal mucosa (fecal matter) and the microbiome, noting the safety and ethical nuances associated with FMT (28:00).
Study: Autism and microbiota transfer therapy
Holingue outlines an FMT study by Kange et al. (2019) in which parents collected stool samples and recorded symptoms during treatment (35:12). Microbiome results showed that autism gut bacteria were less diverse at baseline but increased throughout the treatment, ending with a similar composition to controls. Some long-term effects were recorded (35:20). There was a significant correlation between changes in GI composition and autism behaviors, meaning that as GI symptoms improved, associated behaviors decreased. The treatment was generally well tolerated, with few temporary adverse effects (36:16). The speaker discusses study limitations, including a lack of a placebo group and randomization (37:20). She considers the difficulty and importance of disentangling treatment effects from other drivers and notes the small sample size in this study (38:10).
Recognizing and treating GI issues in autism
The presenter briefly discusses symptoms and signs of GI distress in autism (39:55). She underscores that children, in general, have difficulty communicating pain and that this is often exacerbated in children with neurodevelopmental conditions (41:00). Holingue discusses a recent analysis that found that symptom estimates vary according to how they are measured (i.e., parents/practitioners/complex data) and that existing measurements were not developed for the autistic population (41:44).
Parents are often relied on to detect GI problems in their children. The presenter lists some tell-tale signs of GI distress in autistic children and asserts the need for assessment tools specific to GI experiences in autism (42:35). She outlines the Gastrointestinal and Related Behaviors Inventory (GIRBI), which assesses symptoms, bowel movements, and other behaviors potentially related to GI issues (44:24). Results from the pilot GIRBI questionnaire show high convergent validity, high sensitivity in predicting parent-report diagnosis, and a 7-factor solution to recognizing GI issues in autism (45:40).
Future directions
The speaker asserts that future work on GI measurements should include multiple versions of the GIRBI, with specific attention given to adults and older adults with autism. Future assessments should also incorporate biospecimens with report measures and include self-reports, caregiver reports, and more clinical evaluations (45:50). Holingue provides thanks and acknowledgments (47:12) before the Q&A, where she discusses food allergies, gluten vs. celiac, recommended diets, advocacy in medical settings, and how modes of delivery impact an infant’s gut (47:45).
The speaker:

Take the knowledge quiz
Can’t see the quiz below? Take it online HERE
Editorial – Fecal Microbiota Transplantation and Autism
Over the past several years, Fecal Microbiota Transplantation (FMT) has become the subject of growing interest in the autism community due, at least in part, to the increased awareness of the gut-brain
The Gut, Autism, and Mental Health
Dr. Calliope Holingue, MPH, Ph.D., provides an overview of the intersection between the gut, autism, and well-being. She outlines recent studies on the GI needs and experiences of autistic individuals and
New multi-national study adds to evidence linking alterations of the gut microbiome to autism
Strong new evidence linking alterations of the gut microbiome to autism spectrum disorders (ASD) comes from a new multi-national study by James Morton and colleagues. In the study, researchers in North America,
Constipation in infancy associated with higher likelihood of autism diagnosis
More evidence linking autism spectrum disorders (ASD) to gastrointestinal problems comes from a study by researchers in Taiwan and the United States, who report that ASD occurs at an elevated rate in
Microbiota therapy may lead to lasting beneficial changes in the gut health of children with autism
Microbiota transfer therapy (MTT) may lead to long-term improvements in the gut health of children with autism spectrum disorders (ASD), according to a recent study by Khemlal Nirmalkar and colleagues at Arizona
Gastrointestinal Symptoms in Autistic Patients
In this joint presentation with the World Autism Organization, Frederico Balzola, MD, discusses the intersection of chronic inflammation, gastrointestinal issues, and autism. He considers intestinal permeability and how the microbiome interacts