Over the last decade or so, researchers have begun to look deeply into the gut-brain connection. It may seem obvious that what happens in the brain can affect the gut, as the brain sends signals to all parts of the body. However, what happens in the gut may also affect the brain. Researchers are investigating the implications of this gut-brain connection for individuals with autism.
How are the gut and the brain connected?
The human body comprises only about 25,000 genes. However, the human body has 300 billion bacteria (the microbiome), which live in us and express 100 times more genes than we do. In short, an individual is made up of the combined human genome and the microbiome.
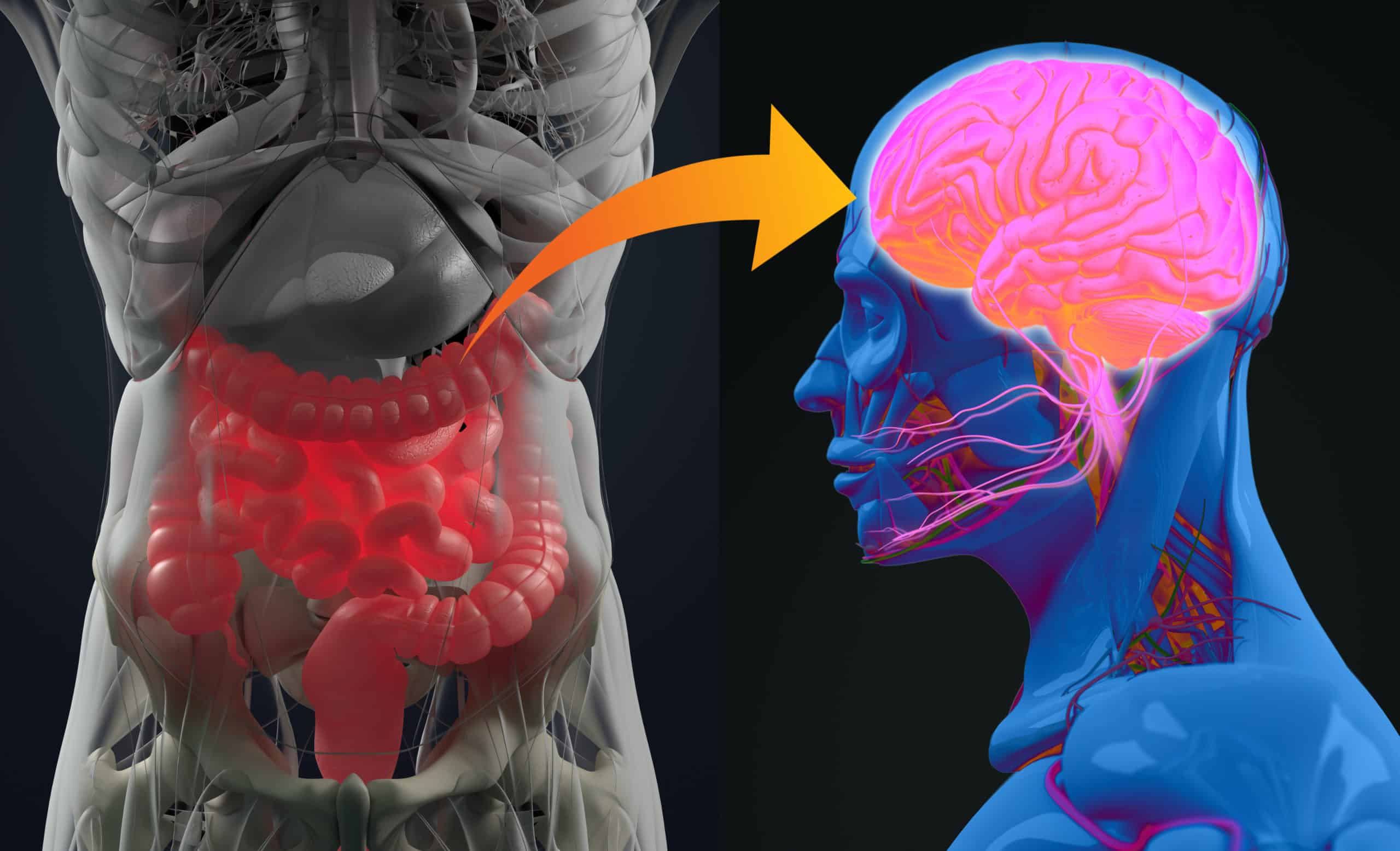
The core of the microbiome resides in the GI tract, which also plays an integral role in the human immune system. This means that what happens in the GI tract can trigger immune responses that can affect the whole body. Researchers are investigating how interactions between gut bacteria and the immune system may impact many diseases and disorders, including cancers, tuberculosis, and autism.
The stress response has also been correlated with GI problems in studies, implying that what happens in the brain affects the gut.
The gut-brain connection and autism
Gastrointestinal symptoms are common in individuals with autism. How common is hard to say. Numbers for individual GI symptoms range from as low as 2% to as high as 95%. This wide range likely due to the fact that GI assessments are done clinically with no single questionnaire or assessment to identify GI issues.
Constipation can be common. 42.5% of study participants met the criteria for functional constipation (Ferguson et al., Autism Res., 2017) in a research project at the University of Michigan. Several studies have found a correlation between GI symptoms and stress, anxiety, increased rigid-compulsive behavior, and irritability or agitation in individuals with autism. (Peters et al., 2014)
Researching the gut-brain connection
The autonomic nervous system
Some studies have focused on the autonomic nervous system. This system is divided into the parasympathetic nervous system, which governs the rest and digest process, and the sympathetic nervous system regulates the fight for flight response. When the sympathetic nervous system is activated, the body is in a stressed state. When the parasympathetic system is active, the body and brain relax.
The autonomic nervous system balances between fight or flight and rest and digest. Both systems are vital, but overactivity in one can cause issues throughout the brain and body. In many people with autism, the sympathetic nervous system is more activated. The body spends more time in a heightened state of anxiety.
In the study, Psychophysiological associations with gastrointestinal symptomatology in Autism Spectrum Disorder (Ferguson, 2017), researchers used heart rate variability to measure sympathetic and parasympathetic balances. In individuals with autism who also have anxiety, their heart rate variability response is altered. This can increase the impact of GI symptoms. The presence of co-occurring anxiety disorder alters the lower GI tract-parasympathetic nervous system relationship.
Another study found that these symptoms tend to manifest as aggression in younger kids, while older individuals have more internalizing symptoms like anxiety and nausea. These responses are compounded when the individual is non-verbal or minimally verbal individuals may be experiencing pain or discomfort and are unable to communicate about the issue.
The importance of diet
Some research has raised the possibility that some individuals with autism have increased amounts of antibodies against gluten. The level of these gluten-targeting antibodies is higher than in siblings or in a control group. Children with both autism and GI symptoms have higher levels of these antibodies compared to kids with autism who do not show GI symptoms.
Alessio Fasano, M.D., has investigated crosstalk between brain and gut and whether it is clinically relevant to autism. Their goal is to define the biology of gastrointestinal dysfunction in ASD to ultimately provide novel personalized treatments. Dr. Fasano expects that a change in the composition of bacteria will instigate Zonulin release, which will cause an intestinal leak, resulting in the uncontrolled passage of elements from the environment into the intestines triggering an immune response. The resulting collateral damage may trigger GI symptoms. He expects that some of the cells will leave the intestine and go to other parts of the body, including the brain, and cause inflammation.
Watch Dr. Alessio Fasano’s full talk on the Cross-Talk Between the Gut and the Brain in ASD.
Exploring the efficacy of Gluten-Free/Casein-free diets
Diets that avoid certain proteins, including gluten and casein, have been the subject of much debate. According to papers published in 2016 and 2017, there is not enough evidence to recommend a gluten/casein-free dietary approach. However, researchers and dietitians are still investigating these potential treatments. Some have pointed out the need to identify children who are most likely to be helped by these diets rather than attempting to apply them to every individual with autism (Elder et al., 2015).
Other treatments under investigation
Several treatments are currently being investigated by researchers that might impact GI symptoms in individuals with autism.
- Probiotics/prebiotics – live bacteria and yeasts that can be consumed before or after eating to assist in balancing the microbiome
- Medications – Various physician-prescribed medications may help address GI and immune system issues.
- Transcutaneous Vagus Nerve Stimulation (tVNS) – stimulates the parasympathetic nervous system to activate the “rest and digest” signal. This is a non-invasive way to modulate the sympathetic nervous system’s responses.
- Gluten-Free/Casein-free diet – despite debates over efficacy, anecdotal evidence shows that these diets may help some individuals.
Most researchers agree that finding the right treatment starts with understanding if there is an imbalance and what kind of imbalance. Ultimately, the choice of treatment will depend on the individual’s symptoms, needs, and comorbidities. Parents, caregivers, and individuals with autism should consult a qualified healthcare professional before embarking on any treatment regimen.
Learn About The Role of Neurotransmitters in GI Disorders Related to Autism
Learn about research exploring the role enteric neurotransmitters, specifically serotonin and oxytocin, play in enteric nervous system (ENS) development and how, when signaling of either of these neurotransmitters is abnormal, it can result in intestinal inflammation and/or motility dysfunction. Presented by Kara Gross Margolis, M.D.
Research Updates: GI Symptoms & Behavior
Free webinar at 1 p.m. Eastern time (US), Wednesday, November 20, 2024 About the speaker: Dr. Bradley Ferguson, PhD is an Assistant Research Professor, MU School of Medicine.
Disordered Eating and Autism – Obesity
Free webinar at 1 p.m. Eastern time (US), Wednesday, October 23, 2024 Tune in to learn research updates on co-occurring disordered eating and autism, including emerging findings to a
Research Updates: Nutrition and Autism 2023
Kelly Barnhill, MBA, CN, CCN, summarizes emerging research on nutritional approaches and supports for autistic people. She outlines recent investigations on sensory processing and nutrition, dietary changes, and supplementation. The speaker
More findings point to high rate of vitamin D deficiency in children with autism
A new study from the Netherlands adds to evidence that vitamin D deficiency is common in children with autism spectrum disorder (ASD). Jet Muskens and colleagues measured the body mass index
Study points to possible role of microbial metabolite in ASD
A new study adds to evidence that alterations of the gut microbiome may play a key role in autism spectrum disorders (ASD). Noting that urinary and fecal levels of the microbial
The Role of Neurotransmitters in GI Disorders Related to Autism
Kara Gross Margolis, MD, explores recent studies surrounding the role of serotonin and the more extensive gut microbiome in gastrointestinal (GI) and inflammatory conditions related to autism. She presents case studies highlighting







